
Diagnostic value of different urine tests for urinary tract infection: a systematic review and meta-analysis
Introduction
Urinary tract infection is a common nosocomial infection. Many factors contribute to the development of urinary tract infection, such as lengthy indwelling catheter time or untimely treatment of the infection. Diagnosis of urinary tract infection cannot rely on clinical symptoms alone and should be combined with biochemical test results to effectively determine the infection site and allow for targeted treatment in order to promote patient recovery (1). If urinary tract infection is not treated effectively, the infection will become chronic, which can have a serious impact on a patient’s health and quality of life (2). Routine urine dry chemical testing is favored by the majority of doctors and is often used in clinical practice due to its rapid and efficient results (3-5).
If urinary tract infection occurs more than 3 times in 1 year, it can be characterized as a recurrent urinary tract infection. Recurrent urinary tract infection is a persistent disease of the urinary system that seriously affects quality of life. Currently, clinical treatment of recurrent urinary tract infection is difficult, and there is an urgent need to improve the level of diagnosis and treatment (6). Recurrent urinary tract infection requires timely and standardized treatment to actively improve the cure rate (7). The pathogens of urinary tract infection are bacterial, but the main pathogenic bacteria have yet to be defined. Antimicrobial drugs are the front-line treatment for urinary tract infection. However, as many patients are prescribed broad-spectrum antibiotics, differing degrees of drug resistance have developed in the population, leading to a significant reduction in drug effectiveness. Therefore, it is necessary to actively analyze the distribution of pathogenic bacteria in patients with recurrent urinary tract infection and explore the sensitivity of pathogenic bacteria to commonly used antimicrobial drugs so as to develop more reliable treatments (8).
Existing tests for urinary tract infections: (I) Urinary routine is a very important basic examination in clinical practice, especially in the diagnosis of urinary tract infection, which has the advantages of simple operation, fast price and low price, and can be accepted by the majority of patients, and this diagnosis method has high diagnostic accuracy. Urine routine has a high frequency of application in clinical practice, which can effectively diagnose a variety of diseases. (II) Urography: Lead to urinary tract infection pathogens types varied, if it is n/med tuberculosis bacterium infection, then completes the urinary tract imaging examination is very important, and want to make the diagnosis on the basis of more powerful, so should also be ultrasound examination, the urinary system can discover whether urinary tract obstruction or whether any stones, better able to analyze the type of urinary tract infection. (III) CT: This examination can find the lesion of urinary tract infection very well. This examination method can better understand the whole process of the lesion in detail, which is of high value for the diagnosis of urinary tract infection.
There are many pathogenic types of recurrent urinary tract infection, including both Gram-negative and relatively low Gram-positive bacteria. Gram-negative bacteria consist of Escherichia coli, Pseudomonas aeruginosa, with each strain accounting for about 20% to 60% of the total Gram-negative bacteria. Urinary tract infection is an inflammatory condition caused by pathogens invading the urinary tract mucosa and nearby tissues (9). Generally, urinary tract infections are divided into upper urinary tract infections (pyelonephritis) and lower urinary tract infections (cystitis, urethritis), most of which occur in women. When diagnosing urinary tract infection, most practitioners will use a urine dipstick test. However, clinical evidence suggests that this method is not sufficient to complete the diagnosis. Therefore, this paper will explore the different tests used in the diagnosis of urinary tract infection (10).
Lesion changes in the endocrine, circulatory, urinary, and digestive systems are often reflected in the changes of urine biochemical indicators. Current urine analysis methods include visual measurement, physics, chemistry, microscopy, and automatic analysis using urine analyzer instruments. The detection of bacteria, leukocytes, and red blood cells in urinary tract infection can be assessed by sediment microscopy, automated urinalysis, bacterial culture, and routine urine dry chemical methods. The selection of an appropriate urine detection method can provide better evidence for the diagnosis of the disease. Different studies believe that the clinical diagnostic value of different urinary tract tests is different, but some studies have found that the sensitivity and specificity of different urinary tract tests are not different, and there are certain controversies. In this study, meta-analysis was used to compare the effectiveness of multiple urine analysis detection methods. We present the following article in accordance with the PRISMA-DTA reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-22-65/rc).
Methods
Search strategy
The PubMed, Embase, Cochrane Library, SpringerLink, Web of Science databases were searched from inception to December 2021. The search keywords were “Bacterial culture”, “Urine sediment microscopy”, “Urinalysis”, “Urine routine dry chemistry”, “Urography”, “CT of urinary system” and “Infection”, and free words respectively. In order to avoid bias caused by language limitations, this study searched English. In order to avoid missing relevant studies, relevant references listed in the article and conference abstracts found in the search were traced (Figure 1).
Inclusion criteria
The inclusion criteria were as follows: (I) The study type was a diagnostic test. (II) The study subjects were bacterial culture, urine sediment microscopy, automated urinalysis, and urine routine dry chemistry used to detect bacteria, leukocytes, and red blood cells. (III) Full text was available and true positive (TP), false positive (FP), false negative (FN), and true negative (TN) values could be directly obtained or calculated from the diagnostic test data. (IV) Inclusion criteria for inclusion studies should be clarified using PICOS criteria.
Exclusion criteria
The exclusion criteria were as follows: (I) The research subjects and study type did not meet the inclusion criteria after reading the title and abstract. (II) The diagnostic test data could not be directly obtained or extracted from the document. (III) The document had incomplete data. (IV) Evaluation indicators were not related to this study.
Evaluation criteria for literature quality
Two reviewers used the Jadad rating scale to independently evaluate 14 studies, mainly to evaluate the randomized controlled experimental design of the included literature. The quality assessment of diagnostic accuracy studies (QUADAS) scale, was used to evaluate the quality of the literature. The QUADAS scale has 14 assessment indicators, and each indicator is evaluated as “yes”, “no”, or “uncertain”. These indicators assess bias (indicators 3, 4, 5, 6, 7, 10, 11, 12, and 14), variation (indicators 1 and 2), and quality (indicators 8, 9, and 13). As the evaluation standard for diagnostic tests, items 3, 8, and 9 of the 14 criteria can be used as optional evaluation indexes. The 14 evaluation indexes are listed together in our study.
The QUADAS assessment of the 14 documents included in this meta-analysis showed that the test results, except the difficult interpretation of the disease spectrum and the reports of the 3 withdrawal cases, were not outstanding (Figure 2).
Analysis of data
Data extracted from the diagnostic tests included TP (gold standard and diagnostic test are positive), FP (diagnostic test is positive and gold standard is negative), FN (diagnostic test is negative and gold standard is positive), and TN (gold standard and diagnostic test are negative).
Bias analysis
Heterogeneity between studies was assessed using I2 statistics, with 25%, 50%, and 75% representing low, medium, and high heterogeneity, respectively. If I2 was <50% and P was >0.1, a fixed-effect model was used for meta-analysis. If I2 was >50% and P was <0.1 and chi-squared analysis showed study heterogeneity, a random-effects model was used for meta-analysis, and the source of the heterogeneity was analyzed using a subgroup analysis. A sensitivity analysis was conducted, and each included study was removed one by one to see whether the pooled effect values were stable and reliable. As shown in the figure, the main part of the literature included in this study is within the scope of the triangle region, and there is no obvious literature publication bias (Figure 3).
Statistical analysis
Meta-DiSc were used to calculate the sensitivity (Sen), specificity (Spe), positive likelihood ratio (LR+), negative likelihood ratio (LR–), and diagnostic ratio (DOR) of the combined literature and the corresponding 95% CI. The Cochrane Collaboration Center provided Rewiew Manger 5.2 software [Cochrane Information Management System (IMS)] for statistical analysis, and the risk ratio of dichotic variables was adopted. RR and 95% CI were used as compare the diagnostic value of different tests analysis statistics in meta-analysis.
Results
Included studies
A total of 300 relevant documents were collected through the database search, and 195 documents were excluded by reading the title, abstract, full text, and quality evaluation independently. A total of 14 studies (11-24) were finally included (Table 1). In addition, there was no significant publication bias in the literature included in this study.
Table 1
| Study | Age | Gender (male) | Diagnostic criteria | Diagnostic methods | Experimental group (N) | Control group (N) | NOS score | Research type |
|---|---|---|---|---|---|---|---|---|
| Gadalla AAH 2019 | 33.71±12.2 | 41.25% | Urinary depression mirror examination | Urinary analyzer (UF100) | 93 | 72 | 8 | RCT |
| Mitchell KF 2020 | 45.65±13.4 | 69.12% | Urinary depression mirror examination | Urinary analyzer (UF101) | 83 | 60 | 7 | RCT |
| Ganesh R 2019 | 33.12±14.5 | 45.72% | Urinary depression mirror examination | Urinary analyzer (UF102) | 115 | 105 | 8 | RCT |
| Kornfält 2021 | 37.15±14.5 | 44.12% | Urinary depression mirror examination | Routine urine chemistry | 63 | 57 | 8 | RCT |
| Fraile 2020 | 22.85±8.4 | 51.89% | Urinary depression mirror examination | Urinary analyzer (UF102) | 55 | 70 | 8 | RCT |
| Hebert C 2020 | 44.36±10.2 | 63.45% | Urinary depression mirror examination | Routine urine chemistry | 51 | 62 | 7 | RCT |
| Han YQ 2020 | 32.62±12.2 | 78.10% | Urinary depression mirror examination | Routine urine chemistry | 77 | 72 | 9 | RCT |
| Charton F 2020 | 32.61±13.0 | 48.75% | Urinary depression mirror examination | Routine urine chemistry | 76 | 60 | 9 | RCT |
| Gama CRB 2020 | 27.25±14.5 | 59.23% | Urinary depression mirror examination | Routine urine chemistry | 38 | 53 | 7 | RCT |
| Paalanne N 2020 | 36.22±15.2 | 56.22% | Urinary depression mirror examination | Urinary analyzer (UF102) | 61 | 68 | 8 | RCT |
| Cheung DA 2020 | 41.35±8.1 | 53.16% | Germiculture | Urinary analyzer (UF102) | 105 | 97 | 8 | RCT |
| Bafna P 2020 | 37.25±16.0 | 66.34% | Germiculture | Routine urine chemistry | 93 | 74 | 8 | RCT |
| Chaudhari 2020 | 38.51±8.6 | 48.34% | Germiculture | Urinary analyzer (UF102) | 60 | 75 | 9 | RCT |
| Kornfält 2019 | 35.51±8.6 | 58.25% | Germiculture | Routine urine chemistry | 29 | 28 | 9 | RCT |
NOS, Newcastle-Ottawa score; RCT, randomized controlled trial.
Urine leucocyte detection
A heterogeneity test of 4 randomized controlled trials (RCTs) found that the heterogeneity of the selected studies was small and a fixed-effect model could be used for meta-analysis. The results of the meta-analysis showed that there was a significant statistical difference between the urine sediment microscopy group and the urine normalization group in urine leucocyte detection (OR =2.15, 95% CI: 1.29–3.56, P=0.003, I2=19%, Z=2.95; Figure 4).
Urine erythrocyte test
A heterogeneity test of 4 RCT studies found that the heterogeneity of the selected studies was small and a fixed-effect model could be used for meta-analysis. The results of the meta-analysis showed that there was a significant statistical difference between urine the sediment microscopy group and the urine normalization group in urine erythrocyte testing (OR =1.87, 95% CI: 1.13–3.09, P=0.01, I2=0%, Z=2.45; Figure 5).
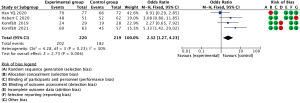
Quantitative determination of urinary protein composition
A heterogeneity test of 4 RCT studies included found that the heterogeneity of the selected studies was small and a fixed-effect model could be used for meta-analysis. The results of the meta-analysis showed that there was a significant statistical difference between the urine sediment microscopy group and the urine normalization group in quantitative determination of urinary protein composition (OR =2.32, 95% CI: 1.27–4.23, P=0.006, I2=30%, Z=2.73; Figure 6).
Determination of urinary enzymes
A heterogeneity test of 4 RCT studies found that the heterogeneity of the selected studies was small and a fixed-effect model could be used for meta-analysis. The results of the meta-analysis showed that there was a significant statistical difference between the urine sediment microscopy group and the urine normalization group in the determination of urinary enzymes (OR =1.67, 95% CI: 1.03–2.72, P=0.04, I2=0%, Z=2.07; Figure 7).
Discussion
Meta-analysis of diagnostic trials is the most accurate source of evidence for clinical decision makers. RCT research still has many deficiencies. Although more and more meta-analyses of diagnostic trials are being published, this has not led to a unified evaluation standard for meta-analysis methodology (25).
Urinary tract infection is a common disease of the urinary system (26), with a higher incidence in females. This difference is attributed to female anatomy, as the female urethral opening is adjacent to the vaginal opening, and the urethra is short and wide. Common urinary tract infection bacteria include Klebsiella, Escherichia coli, and Pseudomonas aeruginosa. Relevant studies have shown that urinary tract infections are mostly caused by a single bacterium. If patients with acute infection do not receive appropriate treatment, chronic infection will occur, leading to decreased quality of life or even renal failure (27). Currently, urine dipstick tests are the most commonly used clinical test in the diagnosis of patients with urinary tract infection, as they are cheap and simple to operate. However, as this test relies on the clinical experience of the doctor and confirmation by microscopy, it is not the most convenient means of diagnosis (28).
Urine culture can be tested separately, but this operation is complicated and easily contaminated by miscellaneous bacteria. In addition, urine culture testing has a high FP rate and it needs to be used for a long time (29-31). Urine dipstick tests and quantitative urine culture often have different results. One study showed that combining the results of these 2 tests can improve the authenticity and accuracy of the diagnosis (32). In the test data, the positive rate (43.7%) was higher than the negative rate (40.6%), and the Spe and Sen of the observation group were significantly higher than those of the control group, with a statistically significant difference (P<0.05) (33). Pinkerton et al. (34) also found that combining the 2 test methods led to a significantly better Spe, Sen, positive predictive value, and negative predictive value than those of the urine dipstick test method alone, thus effectively improving the accuracy and authenticity of diagnosis (35). Because quantitative urine culture takes a long time, a urine dipstick test can be performed first and then confirmed by quantitative urine culture. The combination of these 2 test methods can effectively improve the detection rate and reduce the FP rate.
Our study has some limitations. (I) Due to the small sample size of the studies included here, the conclusions of the meta-analysis may not be generalizable to the larger population. (II) Some outcomes were not eligible for extraction, which affected the number of indicators included. (III) Not do subgroup analysis. Heterogeneity may result from differences and diversity in the inclusion criteria of patients in the studies, interventions, and measures across a range of studies, or from variations in the inherent authenticity of those studies. Statistical heterogeneity is used specifically to describe the degree of variation in effect sizes across a series of studies and to indicate variability between studies except for foreseeable chance.
Our meta-analysis included 14 documents. The small number of documents in the subgroups was mainly due to the diverse testing technologies and instrument models used in various hospitals and the rapid replacement of equipment, which had a certain impact on the homogeneity of screening and inclusion in the study. The results of this study showed that the automated urinalysis and urine dry chemistry methods have good accuracy. However, these methods need to be combined with urine sediment microscopy and urine culture to reach a conclusive diagnosis (36). Therefore, automated urinalysis, urine dry chemistry, and other detection methods can facilitate the early diagnosis, intervention, and treatment of urinary tract infections.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA-DTA reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-22-65/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-22-65/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Thergaonkar RW, Hari P. Current Management of Urinary Tract Infection and Vesicoureteral Reflux. Indian J Pediatr 2020;87:625-32. [Crossref] [PubMed]
- Eremenko R, Barmatz S, Lumelsky N, et al. Urinary Tract Infection in Outpatient Children and Adolescents: Risk Analysis of Antimicrobial Resistance. Isr Med Assoc J 2020;22:236-40. [PubMed]
- Wojno KJ, Baunoch D, Luke N, et al. Multiplex PCR Based Urinary Tract Infection (UTI) Analysis Compared to Traditional Urine Culture in Identifying Significant Pathogens in Symptomatic Patients. Urology 2020;136:119-26. [Crossref] [PubMed]
- Coulthard MG. Using urine nitrite sticks to test for urinary tract infection in children aged < 2 years: a meta-analysis. Pediatr Nephrol 2019;34:1283-8. [Crossref] [PubMed]
- Tornic J, Wöllner J, Leitner L, et al. The Challenge of Asymptomatic Bacteriuria and Symptomatic Urinary Tract Infections in Patients with Neurogenic Lower Urinary Tract Dysfunction. J Urol 2020;203:579-84. [Crossref] [PubMed]
- Selmi I, Azzabi O, Khlayfia Z, et al. Urinary tract infection in the neonates: what radiologic investigations should we do? Tunis Med 2020;98:1005-10. [PubMed]
- Keshi L, Weiwei X, Shoulin L, et al. Analysis of drug resistance of extended-spectrum beta-lactamases-producing Escherichia coli and Klebsiella pneumoniae in children with urinary tract infection. Saudi Med J 2019;40:1111-5. [Crossref] [PubMed]
- Lee AC, Mullany LC, Koffi AK, et al. Urinary tract infections in pregnancy in a rural population of Bangladesh: population-based prevalence, risk factors, etiology, and antibiotic resistance. BMC Pregnancy Childbirth 2019;20:1. [Crossref] [PubMed]
- Villafañe-Ferrer LM, Pinilla-Pérez M, Giraldo-Reyes D, et al. Urinary Tract Infections in College and Non-College Women from Colombia. P R Health Sci J 2019;38:97-101. [PubMed]
- Sime WT, Biazin H, Zeleke TA, et al. Urinary tract infection in cancer patients and antimicrobial susceptibility of isolates in Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. PLoS One 2020;15:e0243474. [Crossref] [PubMed]
- Gadalla AAH, Friberg IM, Kift-Morgan A, et al. Identification of clinical and urine biomarkers for uncomplicated urinary tract infection using machine learning algorithms. Sci Rep 2019;9:19694. [Crossref] [PubMed]
- Mitchell KF, Burnham CD, Gronowski AM. Urinary Tract Infection With Gram-Positive Bacteria Does Not Cause False-Positive Results with the Urine-Based Human Chorionic Gonadotropic Point-of-Care Assay. J Appl Lab Med 2020;5:987-92. [Crossref] [PubMed]
- Ganesh R, Shrestha D, Bhattachan B, et al. Epidemiology of urinary tract infection and antimicrobial resistance in a pediatric hospital in Nepal. BMC Infect Dis 2019;19:420. [Crossref] [PubMed]
- Kornfält Isberg H, Hedin K, Melander E, et al. Uncomplicated urinary tract infection in primary health care: presentation and clinical outcome. Infect Dis (Lond) 2021;53:94-101. [Crossref] [PubMed]
- Fraile Navarro D, Sullivan F, Azcoaga-Lorenzo A, et al. Point-of-care tests for urinary tract infections: protocol for a systematic review and meta-analysis of diagnostic test accuracy. BMJ Open 2020;10:e033424. [Crossref] [PubMed]
- Hebert C, Gao Y, Rahman P, et al. Prediction of Antibiotic Susceptibility for Urinary Tract Infection in a Hospital Setting. Antimicrob Agents Chemother 2020;64:e02236-19. [Crossref] [PubMed]
- Han YQ, Zhang L, Wang JR, et al. Net benefit of routine urine parameters for urinary tract infection screening: a decision curve analysis. Ann Transl Med 2020;8:601. [Crossref] [PubMed]
- Charton F, Conan PL, Le Floch H, et al. Evaluation of pneumococcal urinary antigen testing for respiratory tract infection investigations. Med Mal Infect 2020;50:57-62. [Crossref] [PubMed]
- Gama CRB, Pombo MAG, Nunes CP, et al. Treatment of Recurrent Urinary Tract Infection Symptoms with Urinary Antiseptics Containing Methenamine and Methylene Blue: Analysis of Etiology and Treatment Outcomes. Res Rep Urol 2020;12:639-49. [Crossref] [PubMed]
- Paalanne N, Wikstedt L, Pokka T, et al. Diaper-embedded urine test device for the screening of urinary tract infections in children: a cohort study. BMC Pediatr 2020;20:378. [Crossref] [PubMed]
- Cheung DA, Nicholson A, Butterfield TR, et al. Prevalence, co-infection and antibiotic resistance of Escherichia Coli from blood and urine samples at a hospital in Jamaica. J Infect Dev Ctries 2020;14:146-52. [Crossref] [PubMed]
- Bafna P, Deepanjali S, Mandal J, et al. Reevaluating the true diagnostic accuracy of dipstick tests to diagnose urinary tract infection using Bayesian latent class analysis. PLoS One 2020;15:e0244870. [Crossref] [PubMed]
- Chaudhari PP, Monuteaux MC, Bachur RG. Should the Absence of Urinary Nitrite Influence Empiric Antibiotics for Urinary Tract Infection in Young Children? Pediatr Emerg Care 2020;36:481-5. [PubMed]
- Kornfält Isberg H, Melander E, Hedin K, et al. Uncomplicated urinary tract infections in Swedish primary care; etiology, resistance and treatment. BMC Infect Dis 2019;19:155. [Crossref] [PubMed]
- Doyev R, Ben-Shalom E, Megged O. The predictive utility of prior positive urine culture in children with recurrent urinary tract infections. Eur J Pediatr 2020;179:415-21. [Crossref] [PubMed]
- Frontera JA, Wang E, Phillips M, et al. Protocolized Urine Sampling is Associated with Reduced Catheter-associated Urinary Tract Infections: A Pre- and Postintervention Study. Clin Infect Dis 2021;73:e2690-6. [Crossref] [PubMed]
- Markowitz MA, Monti GK, Kim JH, et al. Rapid diagnostic testing in the management of urinary tract infection: Potentials and limitations. Diagn Microbiol Infect Dis 2019;94:371-7. [Crossref] [PubMed]
- Marsh KJ, Mundy L, Holter JJ, et al. Analysis of urine-specific antibiograms from veterans to guide empiric therapy for suspected urinary tract infection. Diagn Microbiol Infect Dis 2019;95:114874. [Crossref] [PubMed]
- Brookes-Howell L, Thomas-Jones E, Bates J, et al. Challenges in managing urinary tract infection and the potential of a point-of-care test guided care in primary care: an international qualitative study. BJGP Open 2019;3:bjgpopen18X101630.
- Dupont P, Burkhardt W, Boretti F, et al. Urinary tract infections in dogs with spontaneous hypercortisolism - frequency, symptoms and involved pathogens. Schweiz Arch Tierheilkd 2020;162:439-50. [Crossref] [PubMed]
- Betschart C, Albrich WC, Brandner S, et al. Guideline of the Swiss Society of Gynaecology and Obstetrics (SSGO) on acute and recurrent urinary tract infections in women, including pregnancy. Swiss Med Wkly 2020;150:w20236. [Crossref] [PubMed]
- Shimizu T, Sugihara T, Kamei J, et al. Predictive factors and management of urinary tract infections after kidney transplantation: a retrospective cohort study. Clin Exp Nephrol 2021;25:200-6. [Crossref] [PubMed]
- Abbott IJ, van Gorp E, Wijma RA, et al. Efficacy of single and multiple oral doses of fosfomycin against Pseudomonas aeruginosa urinary tract infections in a dynamic in vitro bladder infection model. J Antimicrob Chemother 2020;75:1879-88. [Crossref] [PubMed]
- Pinkerton M, Bongu J, James A, et al. A qualitative analysis of diagnostic testing, antibiotic selection, and quality improvement interventions for uncomplicated urinary tract infections. PLoS One 2020;15:e0238453. [Crossref] [PubMed]
- Schlechter Salinas AK, Hains DS, Jones T, et al. Testing for Urinary Tract Infection in the Influenza/Respiratory Syncytial Virus-Positive Febrile Infant Aged 2 to 12 Months. Pediatr Emerg Care 2019;35:666-70. [PubMed]
- Kaduma J, Seni J, Chuma C, et al. Urinary Tract Infections and Preeclampsia among Pregnant Women Attending Two Hospitals in Mwanza City, Tanzania: A 1:2 Matched Case-Control Study. Biomed Res Int 2019;2019:3937812. [Crossref] [PubMed]








