Surgery is not indicated for the treatment of premature ejaculation
Introduction
There is no debate about the impact premature ejaculation (PE) has on the quality of life of a man (1). Ejaculatory control issues are not a novel concept, having been documented for more than 1,500 years. Today, PE is considered the most common male sexual disorder, affecting as many as 75% of men at some point in their lives (1). A variety of medical options are used to treat PE, and recently various surgical solutions have been introduced (2-10). In this review article, surgical therapy for PE will be closely analyzed in order to determine whether it deserves a place in the treatment of PE.
Medical therapy
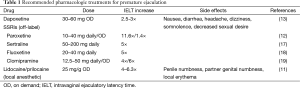
There are currently four key treatments (or therapies) in the pharmacological treatment of PE: topical local anesthetics (LA), selective serotonin reuptake inhibitors (SSRIs), phosphodiesterase type 5 inhibitors (PDE5-I), and tramadol (11-16). The published literature shows topical LA to be moderately effective, increasing intravaginal ejaculatory latency time (IELT) up to 6.3 times (11), but also possibly causing penile hypoesthesia and/or transvaginal absorption, resulting in female anorgasmia. Daily SSRI therapy generates up to an 11.6-fold increase in IELT (12). Dapoxetine, an on-demand, rapid-acting SSRI, approved in 80 countries worldwide but not in the US, leads to a 2.5–3-fold increase in IELT and an overall patient satisfaction of 43% (13). These drugs can have a moderate side-effect profile, including nausea, diarrhea, headache, dizziness, and somnolence, and are seen in up to 60% of patients using dapoxetine as needed (13). Patients are advised not to suddenly halt use of daily SSRIs in order to avoid SSRI discontinuation syndrome (13). Due to the high odds of concomitant erectile dysfunction (ED), many physicians use PDE5-I monotherapy to treat PE, although studies have thus far been equivocal (14). Lastly, tramadol has been shown to effectively delay ejaculation in some men, but has a risk of addiction and other side effects, which are seen in 5% of patients (15). Adherence to medical therapy for PE varies, reaching 70% for dapoxetine, while 30% of patients refused use of off-label SSRI’s, and 30% of those that started discontinued (16). A summary of the recommended pharmacologic treatments for PE is seen in Table 1. Ongoing research is attempting to uncover new techniques for medical management. Patients with PE are currently being recruited in an ongoing clinical study examining the role of onabotulinumtoxinA in the treatment of PE (Allergan, 2015, unpublished data). Current pharmacotherapy has demonstrated efficacy, but additional research is needed to further optimize the management of PE.
Full table
Surgical therapy overview
To date, three surgical approaches have been described: (I) dorsal nerve neurectomy (DNN); (II) hyaluronic acid (HA) gel glans penis augmentation; and (III) circumcision (2-10). These techniques have acquired some popularity in Asia, but have failed to gain acceptance in the rest of the world, in part due to the small number of randomized controlled trials (RCTs), methodological issues such as small sample size, and lack of long-term efficacy and safety data. Key trials in DNN and HA gel glans penis augmentation literature is summarized in Table 2.

Full table
Dorsal nerve neurectomy (DNN)
Some urologists abroad have added DNN to their arsenal in the treatment of PE. According to a nationwide survey of Korean urologists, 73% of urologists reported experience in performing DNN, and almost all private clinicians (94%) felt they were capable of performing the operation (20). Upon review of the existing literature, one might understand why the procedure is gaining popularity. In a Korean RCT in 2012, 78 patients were randomized to either DNN or circumcision and followed for up to 6 months (2). Results showed a 2.7-fold increase in IELT from 1.1 min at baseline to 3.8 min and an increase in perceived control in the DNN group, without any recorded complications. Circumcised patients showed no significant changes in IELT or perceived control after surgery. Similar results have been produced by studies analyzing the effects of pulsed radiofrequency on the dorsal nerve, as well as computed tomography (CT)-guided cryoablation (3,4).
The obvious question is if these studies have been so successful, why have similar procedures not been recommended as treatment for PE in the rest of the world?
First, the literature is lacking long-term data on the safety and efficacy of DNN in the treatment of PE. DNN is an invasive and irreversible procedure, and, to date, the longest studied time point is 6 months after surgery and 1 year after CT-guided cryoablation (2,4). One week after CT-guided cryoablation, the IELT jumped from 55 s at baseline to 256 s, but was only 56% of that value (146 s) after 1 year, demonstrating the importance of long-term follow-up (4). Pulsed radiofrequency neuroablation showed promising results, but patient outcomes were not monitored past 3 weeks of treatment (3). While not detected in the previously described RCT, literature has shown that DNN may lead to certain complications (5). In the previously mentioned Korean national survey, urologists reported that the most common complication of DNN was the recurrence of PE, which they reported to be at approximately 10% (20). Also reported was pain or paresthesia of the glans, penile curvature, ED, and psychotic episodes, amongst others. These significant side effects and complications warrant long-term follow-up before this procedure can be safely recommended.
Another concern with the available DNN literature is the limited sample size of the published studies. The aforementioned RCT did not detail sample size calculations, a requirement for identifying a clinically relevant treatment effect (21). In this study, the small sample size—78 subjects only—undermines the reliability of the findings, particularly that randomization did not perform well, with significant differences in the allocation of study participants to treatment arms; 32 patients (41%) and 46 (59%) for DNN and circumcision, respectively (2). This risk is understandably much more common in studies with a small sample size. This may have drastically reduced the power to detect changes in the IELT in both groups, and limits the application of DNN’s effect to the population at large. On a similar note, the single-center design of this study limits its generalizability. Indeed, practice guidelines should rarely, if ever, be solely based on evidence from single-center trials (22). Because DNN is an invasive and irreversible procedure, urologists and patients can only be convinced of its role in the treatment of PE if favorable results emerge from multicenter, RCTs with large sample sizes and long-term follow-up. Due to these limitations, the International Society of Sexual Medicine (ISSM) has been unable to endorse DNN as an option in the treatment of PE (23). Practicing urologists need to be certain DNN is not only effective, but also safe.
Hyaluronic acid (HA) gel glans penis augmentation
HA gel glans penis augmentation to treat PE has also gained popularity in Asia, albeit at a slower rate than DNN. A survey of Korean urologists predicted that HA gel glans penis augmentation is administered by up to 17% of practicing physicians (20). The principle behind this approach is the injection of a HA gel into the glans penis in order to create a permanent physical barrier between hypersensitive dorsal nerve receptors and the outside environment. As with DNN, initial studies with HA gel glans penis augmentation revealed efficacy, resulting in a 2.9-fold increase in IELT (1.6 to 4.7 min) at 6 months after the procedure, which was maintained when studied 5 and then 10 years later (5,6). When HA gel therapy was compared to DNN, similar delays in IELT were reported, but a higher incidence of complications were seen with DNN or a combination of DNN and HA gel therapy, further detailed in Table 2 (5). Newer reports indicate possible complications including granulomatous foreign body reactions by contaminants and ischemic necrosis due to improper injection technique (7). While somewhat positive, the literature surrounding HA gel glans penis augmentation does not support incorporation into treatment guidelines.
There is a fundamental issue with HA gel therapy being included in the management of PE: there is not a single double-blind RCT in the literature. All trials up to this point have been pilot or prospective observational studies (5,6). Four key factors for associations are at the heart of any clinical study: bias, confounding, chance, and cause (22). With an adequate sample size, a double-blind RCT has the advantage of drastically minimizing the first three variables, making it the best method to determine causality. If the outcome is solely based on the results of observational studies, as observed in the HA gel literature to date, a vulnerable methodology makes it difficult to decipher between what is the result of treatment, and the result of faulty associations. As an example, while the previously described HA gel treatment 5-year follow-up study showed no difference in IELT when compared to immediate post-op IELTs, a more recent pilot study from 2012 documented that the IELT had dropped from 7.71 min post-op to 5.32 min after just three months, demonstrating need for follow-up (8). Additionally, similar to the previous argument against the results with DNN, all studies for HA gel augmentation was conducted in single center institutions, and with a relatively small sample size. If the use of HA gel glans penis augmentation is to be seriously considered as a therapeutic option for PE, then large, multicenter, double-blind RCTs are needed to ensure its safety and efficacy.
Circumcision
The final suggested surgical treatment for PE is actually one of the most commonly performed surgical procedures in the world: circumcision. The prepuce (foreskin) is richly innervated with sensory neurons, explaining the high sensitivity of the human foreskin (24). The precept behind circumcision to treat PE is that the surgical removal of the prepuce also ablates many of these sensory receptors, thus decreasing glans sensitivity. In a systematic meta-analysis exploring the effects of circumcision on male sexual function, the majority of trials showed no improvement in sexual function after the procedure, and it was shown that circumcision may adversely affect sexual function (25). Overall, there were no differences between circumcised and uncircumcised men regarding PE, IELT, ED, low or absent sexual desire, orgasm difficulties and dyspareunia. While some studies showed an IELT delay from 64 to 731 s and reductions in PE frequency from 32% to 14% after circumcision, newer data have discounted these results (9,26). The preponderance of the evidence reveals that there is no significant relationship between post-circumcision mucosal cuff-length and IELT, or brief male sexual function inventory (BMSFI), with some studies even showing a worsening of PE, as well as significant scarring (9). Furthermore, circumcision has been shown to lead to decreased masturbatory pleasure and sexual enjoyment, leading many authors to believe circumcision adversely affects sexual function in a significant number of men (9). While circumcision is commonly performed, the large amount of conflicting data has created widespread skepticism about its role in the treatment of PE.
Of note, some physicians have suggested that a shortened frenulum, which is an elastic band of tissue under the glans, may be linked to PE in up to 43% of patients (10). Surgical lengthening of the frenulum (frenulectomy) has been shown to lead to an average increase in IELT of 2.5 min and improvements in sexual function, but similar to the aforementioned surgical methods, lack of substantial evidence demonstrating safety and efficacy makes it impossible to recommend this surgical treatment for PE (10).
Ethics
The argument against surgical treatment for PE also takes on an ethical context. As medical professionals, one of the maxims of our practice is the principle of non-maleficence. The cornerstone of this concept is to “first, do no harm,” and to avoid even the risk of harm, if at all possible. As we consider invasive and irreversible procedures for a medically manageable condition, it is important to keep this fundamental principle in mind. This discussion applies to the use of DNN for the treatment of PE, as it is already prevalent in Asia. According to a Korean survey of urologists, up to 73% of private clinicians believed that DNN is necessary for the management of patients with PE (20), a disturbing number, considering that the majority of patients do respond to medical management. While not sufficiently studied, DNN can lead to potential complications, thus posing an ethical dilemma. Data on surgical management is limited, and it is difficult, if not impossible, to provide the patient with a “truly informed” consent, when we don’t fully understand the potential risks and benefits of the procedure.
Conclusions
Surgical treatment does not currently have a role in the management of PE. There is a lack of large, multicenter, double-blind RCTs and long-term data to support the safety and efficacy of surgical treatment of PE. With improving medical management, we need to be absolutely convinced that surgery is at least as effective and safe as current medical treatments before we recommend it to patients. As the Dalai Lama wisely stated, “Our prime purpose in this life is to help others. And if you can’t help them, at least don’t hurt them.”
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Symonds T, Roblin D, Hart K, Althof S. How does premature ejaculation impact a man's life? J Sex Marital Ther 2003;29:361-70. [Crossref] [PubMed]
- Zhang GX, Yu LP, Bai WJ, et al. Selective resection of dorsal nerves of penis for premature ejaculation. Int J Androl 2012;35:873-9. [Crossref] [PubMed]
- Basal S, Goktas S, Ergin A, et al. A novel treatment modality in patients with premature ejaculation resistant to conventional methods: the neuromodulation of dorsal penile nerves by pulsed radiofrequency. J Androl 2010;31:126-30. [Crossref] [PubMed]
- David Prologo J, Snyder LL, Cherullo E, et al. Percutaneous CT-guided cryoablation of the dorsal penile nerve for treatment of symptomatic premature ejaculation. J Vasc Interv Radiol 2013;24:214-9. [Crossref] [PubMed]
- Kim JJ, Kwak TI, Jeon BG, et al. Effects of glans penis augmentation using hyaluronic acid gel for premature ejaculation. Int J Impot Res 2004;16:547-51. [Crossref] [PubMed]
- Kwak TI, Jin MH, Kim JJ, et al. Long-term effects of glans penis augmentation using injectable hyaluronic acid gel for premature ejaculation. Int J Impot Res 2008;20:425-8. [Crossref] [PubMed]
- Moon du G, Kwak TI, Kim JJ. Glans penis augmentation using hyaluronic acid gel as an injectable filler. World J Mens Health 2015;33:50-61. [Crossref] [PubMed]
- Abdallah H, Abdelnasser T, Hosny H, et al. Treatment of premature ejaculation by glans penis augmentation using hyaluronic acid gel: a pilot study. Andrologia 2012;44 Suppl 1:650-3. [Crossref] [PubMed]
- Gallo L. Patients affected by premature ejaculation due to glans hypersensitivity refuse circumcision as a potential definite treatment for their problem. Andrologia 2014;46:349-55. [Crossref] [PubMed]
- Gallo L, Perdona S, Gallo A. The role of short frenulum and the effects of frenulectomy on premature ejaculation. J Sex Med 2010;7:1269-76. [Crossref] [PubMed]
- Dinsmore WW, Wyllie MG. PSD502 improves ejaculatory latency, control and sexual satisfaction when applied topically 5 min before intercourse in men with premature ejaculation: results of a phase III, multicentre, double-blind, placebo-controlled study. BJU Int 2009;103:940-9. [Crossref] [PubMed]
- McMahon CG, Touma K. Treatment of premature ejaculation with paroxetine hydrochloride as needed: 2 single-blind placebo controlled crossover studies. J Urol 1999;161:1826-30. [Crossref] [PubMed]
- McMahon CG, Althof SE, Kaufman JM, et al. Efficacy and safety of dapoxetine for the treatment of premature ejaculation: integrated analysis of results from five phase 3 trials. J Sex Med 2011;8:524-39. [Crossref] [PubMed]
- Aversa A, Pili M, Francomano D, et al. Effects of vardenafil administration on intravaginal ejaculatory latency time in men with lifelong premature ejaculation. Int J Impot Res 2009;21:221-7. [Crossref] [PubMed]
- Bar-Or D, Salottolo KM, Orlando A, et al. A randomized double-blind, placebo-controlled multicenter study to evaluate the efficacy and safety of two doses of the tramadol orally disintegrating tablet for the treatment of premature ejaculation within less than 2 minutes. Eur Urol 2012;61:736-43. [Crossref] [PubMed]
- Salonia A, Rocchini L, Sacca’ A, et al. Acceptance of and discontinuation rate from paroxetine treatment in patients with lifelong premature ejaculation. J Sex Med 2009;6:2868-77. [Crossref] [PubMed]
- McMahon CG. Treatment of premature ejaculation with sertraline hydrochloride: a single-blind placebo controlled crossover study. J Urol 1998;159:1935-8. [Crossref] [PubMed]
- Kara H, Aydin S, Yucel M, et al. The efficacy of fluoxetine in the treatment of premature ejaculation: a double-blind placebo controlled study. J Urol 1996;156:1631-2. [Crossref] [PubMed]
- Waldinger MD, Zwinderman AH, Olivier B. On-demand treatment of premature ejaculation with clomipramine and paroxetine: a randomized, double-blind fixed-dose study with stopwatch assessment. Eur Urol 2004;46:510-15; discussion 516. [Crossref] [PubMed]
- Yang DY, Ko K, Lee WK, et al. Urologist's practice patterns including surgical treatment in the management of premature ejaculation: A Korean nationwide survey. World J Mens Health 2013;31:226-31. [Crossref] [PubMed]
- Jepsen P, Johnsen SP, Gillman MW, et al. Interpretation of observational studies. Heart 2004;90:956-60. [Crossref] [PubMed]
- Bellomo R, Warrillow SJ, Reade MC. Why we should be wary of single-center trials. Crit Care Med 2009;37:3114-9. [Crossref] [PubMed]
- Althof SE, McMahon CG, Waldinger MD, et al. An update of the International Society of Sexual Medicine's guidelines for the diagnosis and treatment of premature ejaculation (PE). J Sex Med 2014;11:1392-422. [Crossref] [PubMed]
- Tuncali D, Bingul F, Talim B, et al. Histologic characteristics of the human prepuce pertaining to its clinical behavior as a dual graft. Ann Plast Surg 2005;54:191-5. [Crossref] [PubMed]
- Tian Y, Liu W, Wang JZ, et al. Effects of circumcision on male sexual functions: a systematic review and meta-analysis. Asian J Androl 2013;15:662-6. [Crossref] [PubMed]
- Cortes-Gonzalez JR, Arratia-Maqueo JA, Martinez-Montelongo R, et al. Does circumcision affect male’s perception of sexual satisfaction? Arch Esp Urol 2009;62:733-6. [PubMed]


