
Patient decision-making for surgical treatment of post-prostatectomy stress urinary incontinence: a mixed-methods exploratory pilot study
Highlight box
Key findings
• Among a pilot of men who underwent surgical correction for post-prostatectomy SUI, there were identifiable themes on how men make decisions, evaluate QoL changes and approach treatment options.
• Men value more than being dry with measures of individual success that can include sexual and relationship health.
What is known and what is new?
What is known:
• There is a large number of men living with SUI following treatment for prostate cancer but only a small fraction (~3–6%) are treated.
• Men who delay or choose not to undergo treatment for SUI often regret their decision.
What is new:
• This study begins to shed light on what factors help men make decisions on SUI treatment.
What is the implication, and what should change now?
• Providers managing SUI should go beyond dryness to assess patient goals and refer for SUI treatment sooner.
Introduction
Following surgical treatment for prostate cancer, 10–30% of men will have persistent urinary incontinence (1-3). Even in the era of minimally invasive options and improved surgical techniques, data continue to suggest similar rates of stress urinary incontinence (SUI). Furthermore, older patients with higher comorbidity scores are more likely to experience SUI post-operatively (1,4). Of great concern to patients and providers alike is the impact of SUI on quality of life (QoL), embarrassment, shame, social isolation, and depression (5,6).
Despite the number of men living with SUI following treatment for prostate cancer and large studies that demonstrate excellent safety and high patient satisfaction for surgical treatment for SUI (7-10), only a small fraction (~3–6%) are treated with surgical intervention (11-14). Men who delay or choose not to undergo treatment for SUI have significantly higher levels of decisional regret compared to those who undergo treatment (15). There are therefore men living with untreated incontinence following treatment for prostate cancer whose QoL concerns are not being adequately addressed by current practice patterns.
Much of what is known about the experiences of men with SUI comes from cohorts of men who undergo treatment for prostate cancer or specific treatment for SUI. Men who are living with incontinence after prostate cancer treatment and attempting to navigate when, how, and from whom to seek care for their SUI are relatively understudied. Qualitative analysis is uniquely suited to answer questions regarding patient decision making and lived experience. Broadly, qualitative research involves studying “human experiences and realities, studied through contact with the individual in their natural environments to produce rich, descriptive data that will help us to understand those individual’s experiences” (16). To address the knowledge gap between why men may suffer from severe symptoms but not seek treatment we conducted a pilot study of men seeking care for post-prostatectomy SUI, to capture their objective and subjective experiences and inform development of a qualitative interview guide.
Methods
Study design and patients
Mixed methods were employed to understand the experience of a cohort men living with post-prostatectomy urinary incontinence. Semi-structured interviews, online participant surveys and objective clinical assessment of SUI were performed among a pilot group to guide a future, larger mixed methods study.
Recruitment
Patients were approached as part of a prospective exploratory study of the lived experience of men with SUI. Participants were eligible if they had undergone consultation for SUI at University of California San Francisco between 2015–2017. Recruitment for the interview aimed to include men who had experience with each surgical treatment for male SUI: artificial urinary sphincter (AUS) (“sphincter”, AMS 800™ Boston Scientific Marlborough, MA, USA) and male sling (AdVance XP™ Boston Scientific Marlborough, MA, USA). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Institutional Review Board at the University of California, San Francisco (REF#341528) and informed consent was taken from all individual participants.
Data collection
Semi-structured pilot interviews
Interviews were conducted by trained interviewers (LAH, KQ) by telephone using a minimally structured interview guide to begin to build an outline of possible themes and relevant aspects of the lived experience to inform a future, larger mixed methods study and development of the semi-structured interview guide to be used in that study. Interviews were conducted after participants had been evaluated for SUI and made a treatment decision. Topics of interest for these interviews were identified by the research team and included: patient experience with incontinence, exploring/understanding treatment options for incontinence, treatment decision-making, surgical expectations, and surgical outcomes. The interview guide was expanded and updated throughout the interview process, integrating new, participant-generated topics of interest that emerged through interviews.
Participant survey
After completion of the qualitative interview, participants were asked to complete a brief, online survey aimed to assess the motivational factors that led them to seek treatment for their SUI and to understand which factors were important to them in deciding which treatment choice they made. All study participants had demographic, clinical and patient reported outcome measures (PROMs) collected as per their participation in the quantitative portion of the study. These data and participant survey questions accompany this manuscript as Appendix 1.
Data analysis
After complete transcription of all pilot interviews, 3 coders (NMS, CB, LAH) read all transcripts for themes that emerged using Dedoose, an application for managing, analyzing, and presenting qualitative and mixed method research data (SocioCultural Research Consultants, LLC, Los Angeles, CA, USA). As this was pilot data meant to generate preliminary qualitative data for future study, formal theme analysis and saturation which is well described in qualitative literature was not sought given that this was an exploratory study (17-20).
Results
Fifteen patients were approached to participate in the study and 11 were enrolled with complete information. Four patients had a history of pelvic radiation. Three patients underwent sling and 8 underwent sphincter for management of SUI. The average pads per day decreased from 3.2 to 0.9 following treatment, and patients experienced no surgical complication beyond transient urinary retention in 3 patients (Table 1).
Table 1
| Participant | Age, years | Race/ethnicity | Relationship status | Education level | Pre-surgery pads per day1 | Post-surgery pads per day1 | Prior radiation | Incontinence surgery | New bothersome symptoms | Complication (Y/N) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 74 | White, non-Hispanic | Married | Some college, no degree | 4 | 1 | N | AUS | None | N |
| 2 | 72 | White, non-Hispanic | Married | Some college, no degree | 4 | 0 | N | Sling | >30 days scrotal pain; paresthesia | Y; retention |
| 3 | 78 | White, non-Hispanic | Married | Post graduate or professional degree | >5 | 1 | Y | AUS | >30 days scrotal pain | N |
| 4 | 80 | Decline to answer | Married | Decline to answer | >5 | 1 | N | AUS | None | N |
| 5 | 80 | White, non-Hispanic | Married | Bachelor’s degree | 2 | 1 | N | Sling | Urinary urgency | N |
| 6 | 73 | White, non-Hispanic | Divorced | Bachelor’s degree | >5 | 1 | Y | AUS | None | N |
| 7 | 63 | White, non-Hispanic | Married | Bachelor’s degree | >5 | 0 | N | AUS | Urinary urgency | Y; retention |
| 8 | 82 | White, non-Hispanic | Married | Bachelor’s degree | 4 | 1 | N | AUS | >30 days scrotal pain; urinary urgency | N |
| 9 | 72 | White, non-Hispanic | Married | High school graduate | 2 | 2 | N | Sling | None | N |
| 10 | 74 | White, Hispanic | Married | Vocational training | >5 | 1 | Y | AUS | None | N |
| 11 | 75 | White, non-Hispanic | Married | Post graduate or professional degree | >5 | 1 | Y | AUS2 | Worsening leakage | N |
1, pads per day were characterized from 0–>5, with patients using >1 diaper per day categorized as >5 pads; 2, Participant 11 underwent AUS after already having undergone a “failed” sling which did not improve his continence. AUS, artificial urinary sphincter; sling, male urethral sling; N, no; Y, yes.
Factors influencing the decision to choose surgery
Patient factors that were reported to have a “great deal of influence” vs. “little to no influence” in the decision to pursue surgery are summarized in Figure 1. The factor of greatest significance was individuals’ activities, followed by their urologist, and a sense of embarrassment related to their incontinence. This aligned with how men spoke about their bother in narrative interviews—“I enjoyed walking; I certainly cut back on the amount of walking I did. Secondly, my wife and I we travel a lot, we are both retired and we enjoy travelling abroad, so we go abroad two or three times a year, and we go typically for three weeks—between three and four weeks at a time. So I was finding it, you know, when you go to some third world country or whatever, you don’t know what the hell you gonna be able to buy over there. So I always used to take, you know, at least an average of two pads a day to make sure that was no issue when I was over there” (Participant 5).
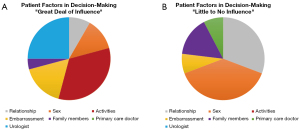
Sex and relationships appeared to be individualized, with some noting that these played a large role in decisions, while others noted little impact from these domains. For example, for one participant sex played a substantial role: “I guess probably it did because as far as like sex life I didn’t feel comfortable at all because of the leakage. I was afraid that I was going to leak. So it definitely affected my decision to proceed with [surgery].” (Participant 6). For other men, such as Participant 8, concomitant ED meant sex was not a major factor in pursuing surgery for SUI—“[A]t that point too I couldn’t get any type of an erection or anything. So we bounced around doing the penile implant and the sphincter valve” (Participant 8).
Factors influencing type of surgery
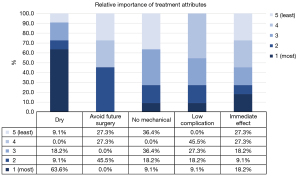
Among our cohort of men, we also examined what factors influenced the type of surgery (sling vs. sphincter) the man chose. Participants were given the structured opportunity to rank 5 considerations (“Being very dry”, “Avoid future surgery”, “Not having a mechanical device that requires manual operation to urinate”, “Fewest number of possible complications”, “Having the surgery be immediately effective”) that impacted their decision to pursue the treatment they chose (Figure 2). All participants highly valued dryness, with only a single participant (who underwent sling surgery) giving “dryness” a score of 4 or 5 (Figure 3). Participants who chose sphincter primarily valued dryness—“I was hoping for no pads a day” (Participant 3). Others were so desperate to be dry that it bypassed other considerations—“I did not give it a second thought because I knew I had to have something done. I did not want to wear a pad all my life… And I figured that he had great success with it. Other people said it had great success, it could work on me. That was it.” (Participant 6). Many sphincter patients also desired avoiding future surgery, which when asked, boiled down to concerns about a sling not being as effective when it came to dryness—“I read a lot of negative stuff on the sling. About all these guys that had surgery to have the sling put in and it didn’t do a thing” (Participant 7). Conversely, men who chose sling mentioned trying to actively avoid a mechanical device—“The fact that is—you got to activate it, you know, physically activate it, unless I misunderstood it, you have to physically activate the thing. And I just—compared to, you know, if the sling was going to work—compared to the sling it just didn’t seem to me the best route to go” (Participant 5). Participant 2 felt similarly—“I had the sling, and then there was that other option of the—it sounds pretty aggressive, they go in and create your own sphincter muscle and you have a little third testicle that you push on and it relieves the bladder. You’d have to be pretty far along to go that route” (Participant 2). In general, participants who chose slings were more variable in their ranking of decisional factors (Figure 2). Complication rate and desire to avoid mechanical device were low priority among participants who underwent sphincter.
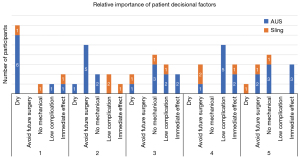
Interestingly, all patients who were candidates for sling and recalled being offered the sling procedure elected to undergo sling. Based on interviews it appeared that the attitude of these men boiled down to: “My notion is to do the sling first. Then, I was really naïve about what it takes to get through surgery at my age. I said ‘If it doesn’t really work the way I think it could work, can we do the sphincter afterwards?’” (Participant 2). Among patients who could potentially derive benefit from a sling, even if the objective degree of incontinence was beyond a likely chance of sling created a ‘cure’ there appeared to be a subset of men who chose this option. The priority of men choosing AUS was a focus on dryness, despite the mechanical device and higher complication rate.
Data were then analyzed to determine the specific weights assigned to various aspects of patient counseling, and are detailed in Figure 3. The relative importance of patient decisional factors, are listed in Figure 2. For the overwhelming majority of patients, most of whom underwent sphincter placement, the factors most important were being dry and avoiding future surgery, whereas the least important factors were complication risk and not having a mechanical device, though the mechanical device factor varied in its importance based on choice of sling or sphincter.
Understanding how patients receive information
Another theme that emerged in the interviews was that the source of information on SUI and treatment was important to men seeking treatment. Patients felt highly variable degrees of comfort with risk and what it meant to be informed. For many patients, hearing information from their physician was crucial and gave them hope—“That’s when [Urologist] said ‘I think we can help you with this. This is what we can offer you. We will be able to do some things for you was the first thing’. I felt so positive the first time I went… I felt really good about that. I was going forward” (Participant 1). “Yeah so. And I thought it was a good idea. Like I said, the way [Urologist] explained it to me, it wouldn’t be a waste. It’d definitely get better” (Participant 10). Others similarly entirely depended on their evaluating urologist—“[B]efore I had my prostate cancer surgery, I talked to a number of people, you know, the various consultants had given me names of people I could talk to discuss why they went that route, etcetera. But I did not do that in this particular incidence. I basically depended on [my surgeon].” (Participant 5). For some men, the availability of information was a relief that there were treatment options that existed, as there was a lack of help from previous urologists—“[My prior Urologist] never gave me one bit of help to be able to go outside in the meantime” (Participant 4). This relief also led to some patients being very eager to undergo surgery even to the exclusion of recognition of risk—“I really didn’t think too much about [risks]. I was just optimistic. I just said ‘I’ve got to have something to get out of these diapers’. Because they tried all sorts of different self applications”. (Participant 9).
In addition to hearing information from physicians, participants noted that they appreciated hearing information on SUI and treatment options from non-physician official channels (e.g., video)—“Well, about the literature and CD that [my Urologist] gave me. [My Urologist] said ‘Go look at this—That’s obviously trying to show you a product and it not telling it like it is’. But he assured me I would be much better off, and I believed him. And I couldn’t be much worse off, so that was the way to go” (Participant 11). Furthermore, some men noted that they appreciated discussing the surgical choices with patients who had experienced it—“I found out that I was going to be able to have the surgery, I called [previous patient] and we discussed it briefly and he had told me that he was down to less than one pad a day on the incontinence and I would have to say right now, I’m still wearing the—I guess I could be personal—I’m still wearing the disposable underwear because I have so many of them. But I’m down to less than one a day too. It’s 98/99 percent leak free” (Participant 3).
Discussion
In this patient-focused exploratory mixed methods study, we identified factors that are relevant for patients considering the decision to pursue surgical treatment for SUI post-prostatectomy, including dryness, immediacy of impact, complications, avoidance of mechanical devices, and necessity for future surgery or intervention. While dryness was the single most important parameter influencing the decision to pursue sphincter surgery, decisions around sling were more variable. In terms of factors that guided the decision to pursue treatment, we found that patient activities (e.g., exercise or social gathering) and discussions with their urologist (including urologist recommendation) were among the most heavily weighted factors in guiding the decision to pursue treatment, whereas sex and relationships had less predictable effects on patients’ decision making.
In this study, all patients who were sling candidates and were offered a sling ultimately chose to pursue that option. These patients were all offered the option to have a sphincter but ultimately valued not having to operate a mechanical device, still having the option of a sphincter if the sling were to be ineffective, and/or having it work right away after surgery. This finding aligns with prior data suggesting that there is likely an unmet demand of patients who are not considered sling candidates or not offered sling who would prefer a sling if offered (12). This finding raises two critical points for urologists; first, it highlights that patient choice is not always directed toward what provides the best chance of dryness, and second, excluding sling from patient choice due to SUI severity or other factors (e.g., radiation) may not be patient-oriented. If patient goals and measures of success differ from that of treating urologists, there may be a benefit to more broadly counseling patients on all options, even those that provide limited chance of dryness.
One interesting finding to highlight is the important weight placed by patients on the urologists’ opinion or recommendation, which was the second-most important factor influencing the decision to pursue surgery. In contrast, primary care physicians, family members, and relationships were not given as much weight. This emphasizes the importance of the urologist-patient relationship, and the significant role urologists play in helping to not only inform patients about their treatment options, but also in guiding the decision to pursue surgery—more-so even than patient’s family members and other clinicians. As a result, clinicians must be aware of this important role.
The national SUI guidelines recognize the complexity of SUI treatment decision-making and advocate “using the shared decision-making model” to discuss treatment options, yet there is no guidance on how urologists should actually do this in practice (21). Shared decision-making is increasingly advocated for, both as an ethical imperative and because there is robust evidence that shared decision-making and patient-centered care actually improve health outcomes (22-26). However, data show that current incontinence counseling may not reliably incorporate shared decision-making (15); in one study that used a shared decision-making assessment scored from 0 (no shared decision-making) to 100 (highest extent of shared decision-making), nearly half of men making decisions about SUI treatment scored shared decision-making below 75 and more than one-fifth scored it below 50. Further, shared decision-making was found to be an independent predictor of decisional regret in multivariable analysis (P=0.001), with lower shared decision-making scores among those with decisional regret. One means of attaining shared decision-making is through decision support tools, which have been shown in rigorous research to improve patients’ knowledge and accuracy of risk perceptions, increase the likelihood of patients making care choices that are congruent with their values, decrease decisional conflict, have a positive effect on patient-clinician communication, and improve satisfaction with decisions and the decision-making process (27). Qualitative data such as those presented here are crucial to drive development of patient-centric decision support tools to improve shared decision-making for SUI.
One of the interesting and underexplored QoL implications of SUI after prostate cancer treatment in our cohort was the role of SUI in sexual and relationship health. For many men in the cohort patient relationships and sex were given the least significance in influencing the decision to pursue for surgery, while activities and embarrassment were some of the most important factors. We suspect this may be due to stigma from the public facing aspects of SUI (e.g., unable to perform activities with friends due to SUI or fear of SUI) compared to the privacy offered by sexual intimacy. This view of a ‘public’ and ‘private’ self as it pertains to men living with incontinence was described nearly 20 years ago and suggests that stigma and embarrassment from SUI can affect both (28). While our cohort did not cite concerns in the ‘private’ domain, there may be significant bother in this domain and it warrants further evaluation with specific questions directed towards this area. It has been previously shown that more than half of men will have arousal incontinence following prostatectomy and that this is worse with increasing SUI severity (29). Furthermore data suggest that address SUI will also improve sexual health metrics (30). The stigma associated with the public-facing impacts of incontinence belie a potentially equally severe, more private experience. Fortunately, timely and appropriate treatment can address both.
There are limitations to our study. Inherent to exploratory studies, there is a small sample size which precludes meaningful statistical analyses. While our study population was inherently heterogenous given that we include men who had undergone both sphincter and sling, we view this as a strength of this pilot study. Given that our goal was to assess whether these methods of data collection could be extrapolated to a larger cohort and to inform development of a semi-structured qualitative interview guide, we sought to recruit a diverse array of patients with varying backgrounds in order to have a representative sample of our patient population and to understand the strengths and limitations of our methods for future studies. An additional limitation is that we focused on recruiting individuals who had undergone surgical SUI treatment in order to understand what influenced the surgical decision-making process. However, this means that we had no insight into the crucial population of men that are evaluated for SUI and chose not to undergo treatment, which propelled us to recruit those men who did not elect surgery into our larger study.
Through this work, we used patient-driven findings to identify what themes and parameters should ultimately be the focus of larger studies that will follow. Our study highlights potential themes to build on with larger studies, including understanding patient priorities, how patients are counseled, and what parameters drive decision-making to pursue surgery (and which surgery). Understanding these parameters can help inform future urologist-patient interactions, guide pre-operative counseling and patient satisfaction measures, and help urologists ultimately serve as better advocates for their patients.
Conclusions
Among a group of 11 men who underwent surgical correction for post-prostatectomy SUI, there were identifiable themes on how men make decisions, evaluate QoL changes and approach treatment options. Men value more than being dry with measures of individual success that can include sexual and relationship health. Furthermore the role of the Urologist remains crucial as patients relied heavily on input and discussion with their Urologist to assist in treatment decisions. These findings can be used to inform future studies of the experience of men with SUI.
Acknowledgments
Funding: This study was supported by National Institute on Aging GEMSSTAR 1R03AG064372-01 (PI: Hampson); National Institute on Aging K24AG054415 (PI: Sudore); NIH/NIDDK K12K083021 (funding: Hampson); Doris Duke Charitable Foundation CTSI – UL1 TR001872 (PI: Hampson); Claude D. Pepper Older Americans Independence Center UCSF Research Education Component Scholar Award (PI: Hampson); and San Francisco Veterans Affairs Medical Center (Hampson, Cooperberg, Sudore, Walter).
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Translational Andrology and Urology for the series “Surgical Management of Stress Urinary Incontinence in Men”. The article has undergone external peer review.
Data Sharing Statement: Available at https://tau.amegroups.com/article/view/10.21037/tau-22-618/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-22-618/coif). The series “Surgical Management of Stress Urinary Incontinence in Men” was commissioned by the editorial office without any funding or sponsorship. LAH served as the unpaid Guest Editor of the series. LAH received grant funding and salary support to conduct this research. LAH held paid and unpaid leadership positions unrelated to this research, as well as received speaker’s honoraria for a talk that was on the same topic as this research but was not directly related to this manuscript. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of University of California, San Francisco (REF#341528) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Novara G, Ficarra V, D'elia C, et al. Evaluating urinary continence and preoperative predictors of urinary continence after robot assisted laparoscopic radical prostatectomy. J Urol 2010;184:1028-33. [Crossref] [PubMed]
- Resnick MJ, Koyama T, Fan KH, et al. Long-term functional outcomes after treatment for localized prostate cancer. N Engl J Med 2013;368:436-45. [Crossref] [PubMed]
- Stanford JL, Feng Z, Hamilton AS, et al. Urinary and sexual function after radical prostatectomy for clinically localized prostate cancer: the Prostate Cancer Outcomes Study. JAMA 2000;283:354-60. [Crossref] [PubMed]
- Hampson LA, Cowan JE, Zhao S, et al. Impact of age on quality-of-life outcomes after treatment for localized prostate cancer. Eur Urol 2015;68:480-6. [Crossref] [PubMed]
- Herr HW. Quality of life of incontinent men after radical prostatectomy. J Urol 1994;151:652-4. [Crossref] [PubMed]
- Bauer RM, Gozzi C, Hübner W, et al. Contemporary management of postprostatectomy incontinence. Eur Urol 2011;59:985-96. [Crossref] [PubMed]
- Berge V, Thompson T, Blackman D. Additional surgical intervention after radical prostatectomy, radiation therapy, androgen-deprivation therapy, or watchful waiting. Eur Urol 2007;52:1036-43. [Crossref] [PubMed]
- Nelson M, Dornbier R, Kirshenbaum E, et al. Use of Surgery for Post-Prostatectomy Incontinence. J Urol 2020;203:786-91. [Crossref] [PubMed]
- Gupta S, Ding L, Granieri M, et al. Utilization of surgical procedures and racial disparity in the treatment of urinary incontinence after prostatectomy. Neurourol Urodyn 2016;35:733-7. [Crossref] [PubMed]
- Kim PH, Pinheiro LC, Atoria CL, et al. Trends in the use of incontinence procedures after radical prostatectomy: a population based analysis. J Urol 2013;189:602-8. [Crossref] [PubMed]
- Bretterbauer KM, Huber ER, Remzi M, et al. Telephone - delivered quality of life after 365 male stress urinary incontinence (SUI) operations. Int Braz J Urol 2016;42:986-92. [Crossref] [PubMed]
- Kumar A, Litt ER, Ballert KN, et al. Artificial urinary sphincter versus male sling for post-prostatectomy incontinence--what do patients choose? J Urol 2009;181:1231-5. [Crossref] [PubMed]
- Gozzi C, Becker AJ, Bauer R, et al. Early results of transobturator sling suspension for male urinary incontinence following radical prostatectomy. Eur Urol 2008;54:960-1. [Crossref] [PubMed]
- Rehder P, Gozzi C. Transobturator sling suspension for male urinary incontinence including post-radical prostatectomy. Eur Urol 2007;52:860-6. [Crossref] [PubMed]
- Hampson LA, Suskind AM, Breyer BN, et al. Predictors of Regret among Older Men after Stress Urinary Incontinence Treatment Decisions. J Urol 2022;207:885-92. [Crossref] [PubMed]
- Nursing Research: A Qualitative Perspective - Patricia L. Munhall - Google Books n.d. Available online: https://books.google.ws/books?id=A16IJw8jstQC&printsec=copyright#v=onepage&q&f=false (accessed January 7, 2023).
- Bradley EH, Curry LA, Devers KJ. Qualitative data analysis for health services research: developing taxonomy, themes, and theory. Health Serv Res 2007;42:1758-72. [Crossref] [PubMed]
- Saldaña J. The Coding Manual for Qualitative Researchers. Sage Publications Ltd.; 2021:440.
- Analyzing Qualitative Data 4 Thematic coding and categorizing 2007. Available online:
10.4135/9781849208574 10.4135/9781849208574 - Michel J, Ballon J, Connor SE, et al. Improving Shared Decision Making in Latino Men With Prostate Cancer: A Thematic Analysis. MDM Policy Pract 2021;6:23814683211014180. [Crossref] [PubMed]
- Sandhu JS, Breyer B, Comiter C, et al. Incontinence after Prostate Treatment: AUA/SUFU Guideline. J Urol 2019;202:369-78. [Crossref] [PubMed]
- Frosch DL, Moulton BW, Wexler RM, et al. Shared decision making in the United States: policy and implementation activity on multiple fronts. Z Evid Fortbild Qual Gesundhwes 2011;105:305-12. [Crossref] [PubMed]
- Légaré F, Adekpedjou R, Stacey D, et al. Interventions for increasing the use of shared decision making by healthcare professionals. Cochrane Database Syst Rev 2018;7:CD006732. [PubMed]
- Greenfield S, Kaplan S, Ware JE Jr. Expanding patient involvement in care. Effects on patient outcomes. Ann Intern Med 1985;102:520-8. [Crossref] [PubMed]
- Guadagnoli E, Ward P. Patient participation in decision-making. Soc Sci Med 1998;47:329-39. [Crossref] [PubMed]
- Stewart M, Brown JB, Donner A, et al. The impact of patient-centered care on outcomes. J Fam Pract 2000;49:796-804. [PubMed]
- Stacey D, Légaré F, Lewis K, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev 2017;4:CD001431. [Crossref] [PubMed]
- Paterson J. Stigma associated with postprostatectomy urinary incontinence. J Wound Ostomy Continence Nurs 2000;27:168-73. [PubMed]
- Bach PV, Salter CA, Katz D, et al. Arousal Incontinence in Men Following Radical Prostatectomy: Prevalence, Impact and Predictors. J Sex Med 2019;16:1947-52. [Crossref] [PubMed]
- Friedl A, Bauer W, Rom M, et al. Sexuality and erectile function after implantation of an Adjustable Transobturator Male System (ATOMS) for urinary stress incontinence. A multi-institutional prospective study. Arch Ital Urol Androl 2016;87:306-11. [PubMed]


