Enhanced ambulatory male urethral surgery: a pathway to successful outpatient urethroplasty
Introduction
In the United States, a concerted effort has been made to reduce healthcare-associated financial burden due to the Affordable Care Act and a rising age of the American patient population (1,2). With the average cost per night of stay in the hospital ranging $1,070 to $3,599 (3), significant cost reduction can be achieved with outpatient surgery.
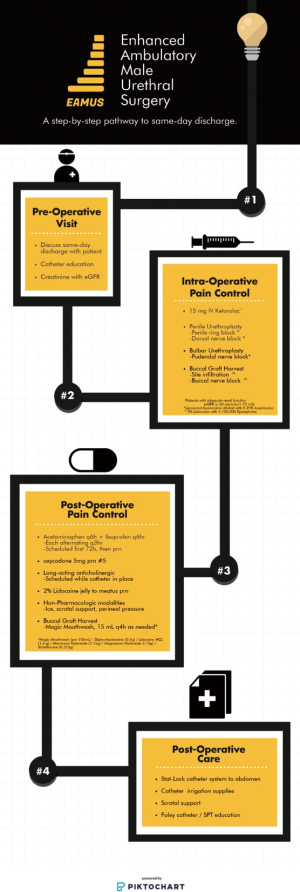
Through a multimodality approach targeting preoperative counseling and postoperative pain management, considerable progress in length of stay following anterior urethroplasty (AU) surgery has been made. This is reflected in National Surgical Quality Improvement Program (NSQIP) data showing a trend from inpatient to outpatient AU surgery over the past two decades (4). Review of NSQIP data from 2003 to 2016 showed the percentage of AU surgery being performed in an inpatient and outpatient setting to be 69.9% and 31.9%, respectively (4,5). MacDonald et al. created a linear regression model revealing a reduction of inpatient stays with mirrored increase in same-day surgery between 2014 and 2016 (4), suggesting a trend towards limiting the duration of postoperative stay. However, in prior studies, outpatient surgery has been defined as same day discharge and outpatient overnight (observation). While several small retrospective studies have demonstrated similar outcomes between same-day and overnight AU surgery (6-8), there remains a need to prospectively define an appropriate care pathway for these patients. We sought to develop an effective and reproducible protocol for enhanced ambulatory male urethral surgery (EAMUS) to promote same day discharge, reduce postoperative narcotic usage, while maintaining high postoperative patient satisfaction rates without a compromise in urethroplasty outcomes.
Methods
We queried our Institutional Board Review approved, prospectively maintained database to identify consecutive patients who underwent same-day AU surgery by a single surgeon (B.R.V) between August 2017 and October 2018 at Mayo Clinic, Rochester, MN. Varying forms of anterior urethroplasty surgery was performed included anastomotic urethroplasty, augmented buccal graft urethroplasty, augmented anastomotic repairs, perineal urethrostomy, and Johansson staged urethroplasty. We utilized EAMUS protocol for perioperative pain management in each case, as depicted in Figure 1 and described below.
Preoperative planning
All patients received formal Foley catheter and/or suprapubic tube education and were counseled to anticipate same day discharge during their preoperative surgery visit. Prior to surgery, each patient underwent retrograde urethrogram (RUG) +/− voiding cystourethrogram (VCUG) for stricture characterization per AUA guidelines (9). Preoperative lab work included a creatinine with eGFR due to the dependence of non-opioid analgesics (Non-steroidal anti-inflammatory drugs) in the perioperative period. Preoperative education included a detailed discussion of the risks and benefits afforded with excision and primary anastomosis versus substitution urethroplasty approaches.
Intraoperative management
A midline ventral penile incision is used for strictures involving the pendulous urethra while a midline scroto-perineal raphae incision is utilized in bulbomembranous stricture repairs. Following completion of perineal cases, oxidized regenerated cellulose (Fibrillar®, Ethicon, Bridgewater, New Jersey) is placed in the periurethral space to aid in hemostasis. If incised, the bulbospongiosus muscle is reapproximated using 2-0 monofilament absorbable suture in a running fashion. Scarpa’s facia is closed using 2-0 monofilament in a running fashion, followed by skin closure using 3-0 monofilament in a running fashion tied at thirds to prevent full incision dehiscence if skin breakdown occurs. We prefer monofilament over alternative braided absorbable suture as it allows 20 days of tensile strength without significant inflammatory response. Following closure, a circumferential penile block is performed in pendulous urethral strictures, while a bilateral pudendal nerve block is performed for bulbomembranous urethral strictures using long acting liposomal bupivacaine (Exparel® Pacira, Parsippany, New Jersey) mixed with 0.25% bupivacaine. Likewise, if a buccal mucosal graft is performed, graft harvest site infiltration and a buccal nerve block are performed using 2% Lidocaine with 1:100,000 epinephrine. All patients with adequate renal function (eGFR ≥60 mL/min/1.73 m2) and no contraindications receive 15 mg of IV ketorolac prior to extubation. Dressing management includes perineal pressure with rolled kerlix, scrotal fluffs, overlying ice pack, and jock strap support system. A 16 Fr silastic Foley catheter with 10 cc in the balloon is used and attached to the patient’s lower abdomen using a Stat-Lock® Foley catheter device (Bard, Covington, Georgia). If a suprapubic tube is present, this is also fixed to the lower abdomen via a Stat-Lock® system.
Post-operative management
Postoperatively, the Foley catheter remains in place for 2–3 weeks after primary repair and 4 weeks in patients with a history of radiation therapy or multiple prior anterior urethroplasties. All patients are instructed on how to perform intermittent irrigation of the catheter(s) using 60 cc normal saline in an as-needed fashion for obstruction.
For the first 72 hours, patients are instructed to take acetaminophen 1,000 mg q 6 hours and ibuprofen 600 mg q 6 hours in an alternating 3-hour fashion as long as no contraindications exist. We provide 5 tablets of oxycodone 5 mg in narcotic naïve patients for break through pain, however, additional tablets may be required if a patient has a history of prior narcotic use. Patients are provided 2% Lidocaine jelly to apply to the tip of the penis as needed for catheter-related discomfort. If not available due to lack of supply or non-coverage by patient’s insurance coverage, bacitracin ointment is substituted. While the catheter is in place, patients are prescribed scheduled oxybutynin extended release 10 mg daily (age <65) or trospium 20 mg twice daily (age ≥65) for bladder spasms. Although over the counter, all patients are provided a prescription for a stool softener to take on a scheduled basis to reduce straining with bowel movements. In our experience, patients are more likely to utilize this class of medication if a prescription is provided.
In patients undergoing buccal graft urethroplasty, the graft site is left open and hemostasis is achieved with needle point electrocautery. Patients are discharged with “Magic Mouthwash”, consisting of diphenhydramine HCL (0.2 g)/lidocaine HCL (1.6 g)/aluminum hydroxide (3.15 g)/magnesium hydroxide (3.15 g)/simethicone (0.315 g).
Following discharge, patients were contacted by telephone within 3 weeks of surgery or evaluated at the time of urinary catheter removal to characterize overall satisfaction with the outpatient experience, satisfaction with post-operative analgesia, and overall percent global function. To assess for overall satisfaction with anesthesia care, patients were asked to rate their experience on a 5 point scale: 1 (not satisfied at all), 2 (somewhat satisfied), 3 (moderately satisfied), 4 (satisfied), and 5 (totally satisfied) (10). Overall satisfaction with postoperative analgesia management was assessed using a 6 point scale as reported by Pavlin et al. (11) which included: 1 (very dissatisfied), 2 (quite dissatisfied), 3 (somewhat dissatisfied), 4 (somewhat satisfied), 5 (quite satisfied), and 6 (very satisfied). Patients rated their average pain score (scale 0–10) during the first 72 hours following discharge as well as the total number of oxycodone 5mg tablets utilized from discharge to the time of survey administration. Lastly, patients were asked to provide their estimated percent global function which is considered the percent of their baseline function at time of survey on a scale of 0–100% (11).
Results
Between August 2017 and October 2018, 57 patients, median age 52.2 years (IQR, 36.3–65.6 years) underwent outpatient same-day AU surgery by a single surgeon (B.R.V.) utilizing our EAMUS protocol (Figure 1). Twenty-six patients (45.6%) underwent excision and primary anastomosis (EPA), median stricture length 2 cm (IQR, 0.95–2.5 cm). Nine patients (15.7%) underwent urethroplasty with buccal mucosal graft (BMG), median stricture length 4 cm (IQR, 2–5.25 cm). The remaining patients (n=22) underwent perineal urethrostomy (n=5, 8%), second stage BMG urethroplasty (n=2, 3%), non-transecting anterior bulbar urethroplasty (n=3, 5%), first stage urethroplasty (n=4, 7%), penile skin flap urethroplasty (n=6, 10%), and other (n=2, 3%).
Primary stricture location included bulbar (n=34, 59.6%), penile (n=20, 35%), and pan-pendulous urethra (n=2, 3.5%) with twelve patients (21%) having a tandem stricture. Stricture etiology was most commonly idiopathic (n=26, 45.6%), iatrogenic (n=6, 10.5%), post-hypospadias repair (n=5, 8.7%), post-catheterization (n=5, 8.7%), and traumatic (n=5, 8.7%). Patient comorbidities included active tobacco smoking (n=8, 14.0%), type II diabetes (n=6, 10.5%), coronary artery disease (n=6, 10.5%), obesity (n=6, 10.5%), and chronic obstructive pulmonary disease (n=2, 3.5%).
Forty-six patients (80.7%) completed the post-surgical assessment including postoperative satisfaction with analgesia, overall outpatient satisfaction, and percent postoperative global function using validated questionnaires (10,11). Median 72-hour post-operative pain score (scale 1–10) was 3 (IQR, 1.75–4) and number of 5 mg oxycodone tablets utilized after discharge was 3.5 (IQR, 0.75–5). Median patient satisfaction with postoperative analgesia (scale 1–6) was 6 (IQR, 5–6) with 43 patients (93.4%) indicating a satisfaction with analgesia score of ≥5 (satisfied to very satisfied). The one patient who reported a score of 2 (somewhat satisfied), had significant concurrent preoperative back pain. No statistically significant effect on analgesia satisfaction score was noted with type of repair, stricture location, stricture length, etiology, postoperative catheter dysfunction, or age of patient, all P>0.05.
A total of 43 patients (93.4%) indicated a score of 4 (satisfied to most satisfied) regarding overall satisfaction with the outpatient experience, including 33 patients (71.7%) reporting a score of 5. The type of repair, stricture location, stricture length, etiology, post-operative catheter dysfunction, and age of the patient did not have a statistically significant effect on overall satisfaction, all P>0.05.
Patients reported a median 30% (IQR, 20–50%) of baseline global function (11) at a median 14 days (IQR, 7–22 days) after surgery. This was most often secondary to catheter discomfort of which 13 of 57 (22.8%) patients reported issues with catheter dysfunction. No statistically significant effect, P>0.05, on percent global function was noted by type of repair, stricture location/length, etiology, post-operative catheter dysfunction, and age of patient.
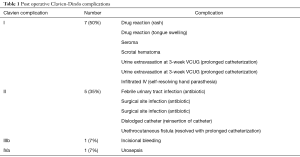
Catheter dysfunction (peri-catheter leakage or obstruction), was common and often resulted in patient phone calls to the surgical service. Six patients (8.9%) made 7 phone calls to our surgical service within 72 hours of discharge. Two patients (3.5%) were reevaluated in the emergency department within 24 hours of discharge. Of these two patients, 1 (1.7%) required readmission. Postoperative complications occurred in 14 patients (24%) ranging from Clavien-Dindo Classification I to IVa (12) (Table 1) with most (85.7%) being considered low grade complications, ≤ II (n=12).
Full table
Discussion
Herein, we have demonstrated that same day discharge following AU surgery can be consistently accomplished if rapid recovery is achieved using the EAMUS protocol. Our findings suggest excellent patient satisfaction with overall outpatient experience and analgesia control with a complication rate comparable to previously published literature.
Preop counseling
We have found that establishing a strong expectation with patients for same day discharge following AU surgery during the preoperative consultation facilitates successful discharge. Certain scenarios may require an overnight stay pending surgical length, timing of completion, and patient age. Patients of advanced aged or with coexisting medical conditions are scheduled as a first case to allow sufficient postoperative recovery time. Those from out of town often feel more comfortable staying in a local hotel in the event they experience post-operative issues; however, repeat evaluation in the emergency department in this cohort was rare and readmission within 24 hours after discharge occurred only once (1.7%).
Catheter education as well as formal urethroplasty education are standard in our presurgical evaluation and is performed by our urology reconstructive team nurse who understands and proactively addresses AU specific concerns regarding catheter care. This eases anxiety of patients and more importantly family members with postoperative catheter care plans.
Historically, patients with substitution urethroplasty were hospitalized or instructed to maintain minimal movement for several days to promote graft imbibition and inosculation (13). With improvements in immediate pain control and adoption of an outpatient algorithm, earlier ambulation risks catheter manipulation and disruption of graft take. As such, we mandate use of the Stat-Lock® foley catheter device which is attached to the lower abdomen to minimize manipulation and movement of the catheter. This remains in place until catheter removal. We prefer fixation to the lower abdomen over the inner thigh to further immobilize the catheter as lower leg adduction and abduction can still produce significant catheter movement if the catheter is secured to the thigh. Depending on the length of urethra and body habitus, this can create a kink in the catheter tubing above the waist line. We circumvent this problem by adding a second Stat-Lock® device on the lower abdomen just medial to the anterior superior iliac spine which forces the tubing into a more obtuse angle and prevents kinking. Occasionally, additional catheter tubing is required. Patients and nurses unfamiliar with our practice may object to the catheter tubing extending above the waist line; however, the drainage bag is still maintained below the level of the bladder ensuring outflow of urine. This again highlights the importance of proactive preoperative catheter education for patients as well as having clear guidelines for outpatient nurses.
EAMUS protocol
Advances in anesthesia protocols have led to a significant reduction in postoperative stay in multiple surgical fields (14,15). Rapid recovery protocols are often based on local pain control with a regional block as the foundation of analgesia (16-20). Similarly, we have found significant success utilizing the EAMUS protocol which includes bilateral pudendal nerve blocks for bulbar urethroplasty, penile ring block with dorsal nerve block for penile urethroplasty, and harvest site infiltration for buccal graft urethroplasty. Early postoperative pain is minimal if the local nerve block is performed correctly. Typically, local pain control with long-acting liposomal bupivacaine (Exparel® Pacira, Parsippany, New Jersey) mixed with 0.25% bupivacaine will last 48 to 72 hours, contributing to early ambulation and excellent patient-reported analgesia. Our surgical cohort demonstrated minimal need for narcotics following discharge after education and implementation of multimodal non-narcotic pain management strategy. As a result, we are able to limit the prescription of narcotic analgesics to 5 tablets of 5 mg oxycodone for those patients without preexisting narcotic requirements.
Post-operative care
Postoperatively our EAMUS protocol focuses on maintaining pain control with non-narcotic analgesics, anticholinergics, lidocaine jelly, and magic mouthwash (for buccal graft harvest) in the first 48 to 72 hours as the effects of liposomal bupivacaine fade. Thus, we find it integral to continue scheduled acetaminophen and ibuprofen on an alternating 3-hour basis for the first 72 hours after which this can be transitioned to an as-needed basis. Likewise, we prefer a scheduled long-acting anticholinergic for bladder spasm management until catheter removal rather than on an as-needed basis. The reason is two-fold as the most common cause of surgical service phone calls in the first 48 hours is related to bladder spasms and leaking around the catheter tubing with sufficient drainage of urine through the tubing. Secondly, reducing the volume of urine expelled around the catheter at the repair site reduces risk of urine infiltration and inflammatory reaction. Catheter discomfort at the meatus and distal penis can be the most significant symptom for some patients in the postoperative setting. Thus, we encourage liberal use of 2% Lidocaine jelly for meatal lubrication and local pain control. Gaps in insurance coverage and intermittent supply by local pharmacies is common, thus substitution with bacitracin ointment can be performed if necessary.
Cases with buccal graft harvest are prescribed “magic mouthwash” consisting of Diphenhydramine HCL (0.2 g)/lidocaine HCL (1.6 g)/aluminum hydroxide (3.15 g)/magnesium hydroxide (3.15 g)/simethicone (0.315 g). Local infiltration of the harvest site and buccal nerve block with 1% lidocaine and 1:100,000 epinephrine in combination with Magic Mouthwash and a soft diet limits patient bother as re-epithelization occurs by 2 weeks.
Patient satisfaction
With the EAMUS protocol, we were able to achieve remarkable satisfaction rates with both the overall outpatient experience as well as the postoperative analgesia management with 71.7% and 65.2% of patients reporting the highest level of satisfaction, respectively. Inclusion of the highest two answers in satisfaction of outpatient experience (satisfied to totally satisfied) captured 93.4% of patients. The remaining three patients answered moderately satisfied (n=2), and somewhat satisfied (n=1). No patients indicated that they were “not satisfied at all”. We anticipate this level of satisfaction with the outpatient experience is directly related to the time and content of the preoperative education visit which reinforces expectations as well as tempers anxiety regarding post-operative care and subsequent discharge.
Our study displays significant satisfaction regarding postoperative analgesia with utilization of the EAMUS protocol. Inclusion of the top two parameters (satisfied to very satisfied) in postoperative analgesic management scales captured 93.4% of patients. This data was further supported with a patient-reported median pain score (scale 1–10) of 3 (IQR, 1.75–4) within 72 hours of surgery. However, this level of control requires a multi-faceted approach that the EAMUS protocol provides. On further review, we found significant underutilization of prescribed oxycodone 5 mg tablets which is a reflection of adequate coverage with non-narcotic options. With opioid overdoses resulting in approximately 50,000 deaths per year in the United States alone (21), optimization and reduction of opioid prescribing patterns is imperative (22).
Safety
Safety of same day discharge anterior urethroplasty has been shown to be similar to inpatient stays in several studies (6,23,24). Our complication rate of 24%, while higher than reported literature, is likely elevated for two reasons. First, accurate capture of complications is more likely with implementation of postoperative surveys. Second, inclusion of postoperative catheter related issues likely augmented our complication rate. Half of all complications (n=7) were Clavien-Dindo Classification I, while 85% were classification ≤ II. Most importantly, duration of stay following surgery should have minimal impact on the incidence of complications. Of the 57 patients, only one patient required readmission within 24 hours of discharge. Despite these findings, we recognize that higher powered, well-organized studies are necessary to further validate similar postoperative complication rates in outpatient versus inpatient settings.
Limitations
Our study is not without limitations including a small cohort single-surgeon case series, no inpatient control group, and innate variability of urethral stricture disease and management. Likewise, we recognize that integral segments of this protocol (i.e., urology reconstructive nurse with dedicated education visit time, etc.) may not be available or financially feasible for all providers. Additionally, our surgical service assisted in administering the survey which could have introduced bias. Lastly, a cost effectiveness model could further solidify the secondary effects related to an expected reduction in healthcare related expenditures with same day discharge. However, we feel that the prospective nature of this study with the utilization of a defined algorithmic pathway (EAMUS) enhanced and streamlined the outpatient AU experience without significant change in postoperative morbidity. Pending long-term urethroplasty success outcomes, these findings suggest that same day surgery should be the new standard of care for the majority of patients undergoing AU surgery.
Conclusions
With careful planning, same day discharge AU surgery can be safely performed in patients with adequate preoperative education. A proactive multi-modal analgesia protocol permits early postoperative ambulation, faster recovery time, and practical discharge timing while maintaining excellent patient satisfaction. Additional higher volume studies with control groups are needed to verify our findings.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved via Mayo Clinic Institutional Review Board (ID: 18-012053) and informed consent was obtained from all patients.
References
- Berwick DM, Hackbarth AD. Eliminating Waste in US Health Care. JAMA 2012;307:1513-6. [Crossref] [PubMed]
- GK V, VA V. The next four decades: The older population in the United States: 2010 to 2050. In: Bureau UC, editor. Washington DC2010. p. 25-1138.
- Association AH. AHA Hospital Statistics. 2018 ed: American Hospital Association; 2018. 272 p.
- MacDonald S, Haddad D, Choi A, et al. Anterior Urethroplasty Has Transitioned to an Outpatient Procedure Without Serious Rise in Complications: Data From the National Surgical Quality Improvement Program. Urology 2017;102:225-8. [Crossref] [PubMed]
- National Surgical Quality Improvement Program 2005. Available online: www.ascsnsqip.org
- Lewis JB, Wolgast KA, Ward JA, et al. Outpatient Anterior Urethroplasty: Outcome Analysis and Patient Selection Criteria. J Urol 2002;168:1024-6. [Crossref] [PubMed]
- Theisen K, Fuller TW, Bansal U, et al. Safety and Surgical Outcomes of Same-day Anterior Urethroplasty. Urology 2017;102:229-33. [Crossref] [PubMed]
- Okafor H, Nikolavsky D. Impact of Short-Stay Urethroplasty on Health-Related Quality of Life and Patient's Perception of Timing of Discharge. Adv Urol 2015;2015:806357.
- Wessells H, Angermeier Keith W, Elliott S, et al. Male Urethral Stricture: American Urological Association Guideline. J Urol 2017;197:182-90. [Crossref] [PubMed]
- Royse CF, Chung F, Newman S, et al. Predictors of patient satisfaction with anaesthesia and surgery care: a cohort study using the Postoperative Quality of Recovery Scale. Eur J Anaesthesiol 2013;30:106-10. [Crossref] [PubMed]
- Pavlin DJ, Chen C, Penaloza DA, et al. A survey of pain and other symptoms that affect the recovery process after discharge from an ambulatory surgery unit. J Clin Anesth 2004;16:200-6. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Riechardt S, Fisch M. Two-stage urethroplasty with buccal mucosa. BJU Int 2012;109:150-62. [Crossref] [PubMed]
- Hoeffel DP, Daly PJ, Kelly BJ, et al. Outcomes of the First 1,000 Total Hip and Total Knee Arthroplasties at a Same-day Surgery Center Using a Rapid-recovery Protocol. J Am Acad Orthop Surg Glob Res Rev 2019;3:e022. [PubMed]
- Stambough JB, Bloom GB, Edwards PK, et al. Rapid Recovery After Total Joint Arthroplasty Using General Anesthesia. J Arthroplasty 2019;34:1889-96. [Crossref] [PubMed]
- Caldwell GL Jr, Selepec MA. Reduced Opioid Use After Surgeon-Administered Genicular Nerve Block for Anterior Cruciate Ligament Reconstruction in Adults and Adolescents. HSS J 2019;15:42-50. [Crossref] [PubMed]
- Kulacoglu H, Yazicioglu D, Ozyaylali I. Prosthetic repair of umbilical hernias in adults with local anesthesia in a day-case setting: a comprehensive report from a specialized hernia center. Hernia 2012;16:163-70. [Crossref] [PubMed]
- Lydiksen HA, Glavind-Kristensen M, Greisen S. High Patient Satisfaction With Local Anesthesia and Light Sedation in a Novel Fast-Track Setup for Sacrospinous Fixation. Female Pelvic Med Reconstr Surg 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Patel MA, Gadsden JC, Nedeljkovic SS, et al. Brachial Plexus Block with Liposomal Bupivacaine for Shoulder Surgery Improves Analgesia and Reduces Opioid Consumption: Results from a Multicenter, Randomized, Double-Blind, Controlled Trial. Pain Med 2019. [Epub ahead of print]. [Crossref] [PubMed]
- Rouholamin S, Jabalameli M, Mostafa A. The effect of preemptive pudendal nerve block on pain after anterior and posterior vaginal repair. Adv Biomed Res 2015;4:153. [Crossref] [PubMed]
- Montandon G, Slutsky AS. Solving the Opioid Crisis: Respiratory Depression by Opioids as Critical Endpoint. Chest 2019;156:653-8. [Crossref] [PubMed]
- Ziegelmann MJ, Joseph JP, Glasgow AE, et al. Wide Variation in Opioid Prescribing After Urological Surgery in Tertiary Care Centers. Mayo Clin Proc 2019;94:262-74. [Crossref] [PubMed]
- Lacy JM, Madden-Fuentes RJ, Dugan A, et al. Short-term Complication Rates Following Anterior Urethroplasty: An Analysis of National Surgical Quality Improvement Program Data. Urology 2018;111:197-202. [Crossref] [PubMed]
- MacDonald MF, Al-Qudah HS, Santucci RA. Minimal impact urethroplasty allows same-day surgery in most patients. Urology 2005;66:850-3. [Crossref] [PubMed]